Introduction: Understanding Low Semen Volume 🔍
Low semen volume, clinically defined as ejaculation of less than 1.5 milliliters of fluid, represents a common concern among men. While sometimes purely cosmetic, reduced ejaculate volume can also indicate underlying health issues or affect fertility in some cases. This comprehensive analysis examines the ten most common causes of low semen volume, providing evidence-based solutions for each factor. By understanding these causes and their remedies, men can address this concern effectively and determine when medical intervention might be necessary.
Semen volume varies naturally between individuals, with normal range typically between 1.5 to 5 milliliters per ejaculation. Various physiological, lifestyle, and medical factors can influence this volume, many of which are modifiable through targeted interventions. This guide explores these causes systematically, offering practical strategies to optimize ejaculatory volume while improving overall reproductive health.
1. Dehydration: The Most Common and Easily Fixable Cause 💧

Dehydration represents perhaps the most straightforward and common cause of reduced semen volume:
How Dehydration Affects Semen Volume
| Hydration Status | Effect on Semen Volume | Mechanism | Prevalence |
|---|---|---|---|
| Mild dehydration (1-2% body weight) | 10-20% volume reduction | Reduced seminal fluid production | Very common |
| Moderate dehydration (3-5% body weight) | 20-30% volume reduction | Significant decrease in all fluid secretions | Common |
| Chronic inadequate intake | Long-term reduction in baseline volume | Adaptive response to conserve fluids | Common in many men |
Evidence-Based Hydration Solutions 🥤
| Solution | Implementation | Expected Timeframe | Success Rate |
|---|---|---|---|
| Increased water intake | 2.5-3.5 liters (10-14 cups) daily | 24-48 hours for initial improvement | High (70-90% report improvement) |
| Hydration timing | 500ml 1-2 hours before sexual activity | Same day effect | Moderate (depends on prior status) |
| Electrolyte balance | Proper sodium/potassium intake | 1-3 days | Supports overall hydration effectiveness |
| Hydration monitoring | Urine color check (pale yellow ideal) | Immediate feedback | Helps maintain optimal hydration |
| Reduced diuretics | Limit caffeine, alcohol before sexual activity | Same day effect | Supports overall hydration status |
The Mayo Clinic confirms that proper hydration affects all bodily secretions, including semen production, making this a crucial first intervention: https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/water/art-20044256
2. Hormonal Imbalances: Testosterone and Beyond 🧪
Hormonal factors play a critical role in semen production and volume:
Key Hormonal Influences on Semen Volume
| Hormone | Role in Semen Production | Signs of Imbalance | Testing Method |
|---|---|---|---|
| Testosterone | Primary driver of reproductive function | Low energy, reduced libido, erectile issues | Blood test (total and free testosterone) |
| Follicle-stimulating hormone (FSH) | Stimulates sperm production | Can be elevated with testicular problems | Blood test |
| Luteinizing hormone (LH) | Stimulates testosterone production | Irregular levels signal pituitary or testicular issues | Blood test |
| Prolactin | Excessive levels can impair function | Reduced desire, erectile dysfunction | Blood test |
| Thyroid hormones | Support overall reproductive function | Fatigue, weight changes, temperature sensitivity | Thyroid panel blood test |
Evidence-Based Solutions for Hormonal Optimization 💉
| Solution | Implementation | Expected Timeframe | Medical Supervision Needed |
|---|---|---|---|
| Medical hormone evaluation | Comprehensive blood panel | 2-4 weeks for results and plan | Yes – endocrinologist or urologist |
| Weight optimization | Achieve healthy BMI through diet and exercise | 3-6 months for significant changes | Recommended |
| Sleep optimization | 7-9 hours of quality sleep nightly | 2-4 weeks for hormonal improvement | No, but tracking helpful |
| Resistance training | 2-4 strength sessions weekly | 4-12 weeks for hormonal benefits | Recommended initially |
| Stress management | Regular stress-reduction practices | 4-8 weeks for hormonal improvement | Beneficial for some techniques |
| Vitamin D optimization | Sun exposure or supplementation if deficient | 8-12 weeks | Yes for supplementation |
| Zinc and magnesium adequacy | Dietary sources or supplementation if deficient | 8-12 weeks | Recommended for supplements |
The Cleveland Clinic provides comprehensive information on male hormonal health and its impact on reproductive function: https://my.clevelandclinic.org/health/articles/15229-male-infertility
3. Frequent Ejaculation: Recovery Time Matters ⏱️
The timing between ejaculations significantly affects semen volume:
Ejaculation Frequency Impact
| Frequency | Effect on Volume | Recovery Pattern | Practical Implication |
|---|---|---|---|
| Multiple times daily | Significant volume reduction (60-80%) | Insufficient recovery time | Not sustainable for volume goals |
| Daily ejaculation | Moderate volume reduction (40-60%) | Partial recovery between ejaculations | Suboptimal for volume concerns |
| Every 2-3 days | Optimal balance for most men | Sufficient recovery without stagnation | Good compromise for regular activity |
| 3-5 day abstinence | Maximum volume for most men | Complete recovery and accumulation | Strategic timing for specific occasions |
| >7 days abstinence | Diminishing returns, potential quality issues | Plateaued volume, decreased sperm quality | Not recommended for most men |
Evidence-Based Management Strategies 📅
| Strategy | Implementation | Benefits | Considerations |
|---|---|---|---|
| Strategic abstinence | 2-5 days before desired maximum volume | 30-50% volume increase | Plan around important occasions |
| Consistent moderate frequency | Every 2-3 days as baseline pattern | Balanced semen parameters | Good for overall reproductive health |
| Recovery tracking | Note volume changes with different intervals | Identifies personal optimal frequency | Individual variation is significant |
| Post-illness recovery | Extended abstinence after illness/stress | Allows full recovery of parameters | Important after significant health events |
Research published in the Journal of Andrology confirms that ejaculatory frequency significantly impacts semen volume, with 2-5 days typically providing optimal results: https://pubmed.ncbi.nlm.nih.gov/16422830/
4. Age-Related Changes: Managing the Inevitable ⏳

Age brings natural changes to reproductive function, including semen volume:
Age-Related Volume Changes
| Age Range | Typical Volume Change | Mechanism | Population Variance |
|---|---|---|---|
| 20-30 years | Optimal baseline volume | Peak reproductive function | Wide natural variation |
| 30-40 years | Minimal reduction (0-10%) | Early hormonal shifts | Some men maintain peak volume |
| 40-50 years | Mild to moderate reduction (10-20%) | Decreasing testosterone, glandular changes | Significant individual variation |
| 50-60 years | Moderate reduction (15-30%) | Hormonal shifts, prostate changes | Health status heavily influences outcomes |
| 60+ years | Significant reduction (25-40%) | Multiple age-related factors | Healthy men may maintain better volume |
Evidence-Based Age Management Strategies 🧓
| Strategy | Implementation | Effectiveness | Scientific Support |
|---|---|---|---|
| Hormonal optimization | Regular testing and medical management | Moderate to high | Strong evidence for hormone-volume connection |
| Prostate health maintenance | Regular check-ups, prostate-supporting nutrition | Moderate | Good evidence for prostate-volume relationship |
| Physical fitness maintenance | Regular resistance and aerobic exercise | Moderate | Strong evidence for exercise-hormone relationship |
| Anti-inflammatory lifestyle | Mediterranean diet, stress management | Moderate | Emerging evidence for inflammation’s role |
| Sexual regularity | Consistent but not excessive sexual activity | Moderate | Supports ongoing reproductive function |
| Adaptive expectations | Understanding normal age changes | N/A | Reduces unnecessary concern over natural changes |
Harvard Health Publishing provides information on normal age-related changes in male sexual function and strategies to maintain optimal health: https://www.health.harvard.edu/mens-health/aging-and-the-male-reproductive-system
5. Medication Side Effects: Pharmaceutical Impacts 💊

Various medications can significantly affect semen volume:
Common Medications Affecting Semen Volume
| Medication Category | Examples | Mechanism of Impact | Reversibility |
|---|---|---|---|
| Alpha-blockers | Tamsulosin (Flomax), Alfuzosin | Can cause retrograde ejaculation | Often reversible upon discontinuation |
| Antidepressants (SSRIs) | Fluoxetine, Sertraline, Paroxetine | Affect ejaculatory function and volume | Usually reversible, may require transition period |
| Antipsychotics | Risperidone, Haloperidol | Hormonal effects, ejaculatory changes | Variable reversibility |
| Anti-hypertensives | Beta-blockers, Calcium channel blockers | May affect ejaculatory function | Usually reversible |
| Antihistamines | Diphenhydramine, Chlorpheniramine | Can thicken secretions, reduce volume | Quickly reversible |
| Opioids (long-term) | Various prescription opioids | Hormonal suppression | May require hormonal recovery period |
| 5-alpha reductase inhibitors | Finasteride, Dutasteride | Reduce prostate fluid production | Usually partially reversible |
| Testosterone replacement | Various formulations | Can suppress natural production | Variable reversibility |
Evidence-Based Management Strategies 👨⚕️
| Strategy | Implementation | Considerations | Medical Supervision |
|---|---|---|---|
| Medication review | Comprehensive review with prescribing physician | Balance necessary treatment with side effects | Required |
| Alternative medications | Explore alternative drugs in same class | Not always possible for all conditions | Required |
| Dose optimization | Adjust dosage to minimize side effects | Must maintain therapeutic effect | Required |
| Timing modification | Take medication at specific times relative to sexual activity | Works for some medication types | Discuss with physician |
| Offset strategies | Implement other volume-enhancing approaches | Can partially compensate for medication effects | Recommended |
| Acceptance when necessary | Understand when medication is essential despite effects | Mental health and serious conditions take priority | Supportive counseling may help |
WebMD provides information about medication side effects on sexual function and appropriate management approaches: https://www.webmd.com/men/features/drugs-men-sex-side-effects
6. Medical Conditions: Underlying Health Factors 🏥
Several medical conditions can directly impact semen volume:
Medical Conditions Affecting Semen Volume
| Condition | Mechanism of Impact | Diagnostic Approach | Prevalence |
|---|---|---|---|
| Retrograde ejaculation | Semen enters bladder rather than exiting penis | Urinalysis after ejaculation | Uncommon but significant |
| Ejaculatory duct obstruction | Blockage prevents normal ejaculation | Specialized imaging, semen analysis | Rare |
| Hypogonadism | Low testosterone reduces reproductive function | Blood tests, physical examination | Moderately common, increases with age |
| Prostate conditions | Inflammation or enlargement affects fluid production | Physical exam, PSA test, imaging | Common in men over 50 |
| Diabetes (uncontrolled) | Nerve damage, ejaculatory dysfunction | Blood glucose testing, comprehensive evaluation | Growing prevalence |
| Post-surgical changes | Prostate surgery, vasectomy affect components | Medical history, physical examination | Depends on surgical history |
| Genetic conditions | Various rare disorders affecting reproduction | Genetic testing, specialized evaluation | Rare |
| Congenital abnormalities | Structural issues present from birth | Physical examination, imaging | Rare |
Evidence-Based Medical Interventions 🩺
| Condition | Treatment Approach | Effectiveness | Medical Specialty |
|---|---|---|---|
| Retrograde ejaculation | Medication (pseudoephedrine, imipramine), surgery in select cases | Moderate | Urology |
| Ejaculatory duct obstruction | Transurethral resection of ejaculatory ducts | High when appropriate | Urology |
| Hypogonadism | Testosterone replacement therapy, other hormonal interventions | High | Endocrinology, Urology |
| Prostate conditions | Condition-specific treatments (medications, procedures) | Variable by condition | Urology |
| Diabetes | Blood sugar control, nerve support nutrients | Moderate prevention, limited reversal | Endocrinology |
| Post-surgical issues | Specialized approaches based on specific surgery | Variable | Urology |
| Genetic conditions | Condition-specific management, assisted reproduction | Variable | Genetics, Reproductive Endocrinology |
The American Urological Association provides comprehensive information on conditions affecting male reproductive health and appropriate treatments: https://www.urologyhealth.org/urology-a-z/l/low-semen-volume
7. Nutritional Deficiencies: Missing Building Blocks 🥑
Specific nutrient deficiencies can significantly impact semen production:
Key Nutrients for Semen Volume
| Nutrient | Role in Semen Production | Signs of Deficiency | Food Sources |
|---|---|---|---|
| Zinc | Essential for prostate function and semen production | Reduced volume, poor immunity | Oysters, meat, pumpkin seeds |
| Selenium | Supports reproductive gland function | Various reproductive parameters affected | Brazil nuts, fish, meat |
| Omega-3 fatty acids | Support hormone production, gland function | Inflammation, reduced reproductive function | Fatty fish, walnuts, flaxseed |
| Vitamin D | Supports testosterone production | Reduced testosterone, lower volume | Sunlight, fatty fish, fortified foods |
| L-Arginine | Precursor for functions affecting semen production | Reduced reproductive parameters | Turkey, chicken, pumpkin seeds |
| B Vitamins | Support energy production and hormonal function | Fatigue, reduced reproductive function | Whole grains, meat, eggs, leafy greens |
| Antioxidants (C, E) | Protect reproductive tissues | Oxidative stress markers | Fruits, vegetables, nuts, seeds |
Evidence-Based Nutritional Interventions 🍽️
| Intervention | Implementation | Expected Timeframe | Effectiveness |
|---|---|---|---|
| Comprehensive nutrient-dense diet | Mediterranean or similar balanced eating pattern | 2-3 months for significant impact | High for nutritionally-deficient men |
| Targeted zinc optimization | Zinc-rich foods or supplement if deficient | 2-3 months | High when deficient |
| Selenium adequacy | 1-2 Brazil nuts daily or other sources | 2-3 months | Moderate |
| Omega-3 increase | Fatty fish 2-3 times weekly or plant sources | 2-3 months | Moderate |
| Vitamin D optimization | Sunlight exposure, food sources, supplement if deficient | 2-3 months | Moderate when deficient |
| Antioxidant-rich diet | 8-10 servings fruits/vegetables daily | 1-2 months | Moderate |
| Professional nutritional assessment | Comprehensive testing with healthcare provider | Varies by findings | High for identifying specific issues |
The Cleveland Clinic provides detailed information on nutrition’s impact on male reproductive health and semen parameters: https://my.clevelandclinic.org/health/articles/15229-male-infertility
Boost Your Semen Volume Naturally with Semenax: The Ultimate Nutritional Solution
How Nutritional Deficiencies Impact Your Semen Production
Lacking essential nutrients directly affects your reproductive health and semen volume. When your body misses critical building blocks, semen production suffers significantly. This is where targeted supplementation becomes vital.
Semenax: Your Complete Nutritional Solution for Enhanced Semen Volume

Semenax delivers 18 powerful natural ingredients specifically formulated to increase semen volume and improve overall reproductive health. Unlike single-nutrient supplements, Semenax provides a comprehensive formula that targets all aspects of semen production.
Directly Nourishes Your Reproductive System
Semenax works by delivering essential nutrients directly to your three primary semen-producing glands:
- Seminal vesicle
- Prostate gland
- Bulbourethral gland
This targeted approach naturally stimulates increased fluid production where it matters most.
Key Nutrients That Restore Optimal Semen Volume
The powerful Semenax formula includes:
- Zinc Aspartate (30mg): Combats zinc deficiency that directly reduces testosterone and sperm health
- L-Carnitine (500mg): Enhances sperm motility and overall reproductive function
- Vitamin E (60IU): Protects sperm cells with powerful antioxidant properties
- Maca (400mg): Scientifically proven to support male fertility and reproductive health
Clinically Proven Results You Can Experience
Men using Semenax consistently report significant improvements in their semen volume. A company-sponsored clinical study revealed an impressive 20% increase in ejaculate volume after just 8 weeks of regular use.
Why Semenax Stands Out for Nutritional Deficiency Issues
What makes Semenax particularly effective is its synergistic approach. Rather than addressing single nutrients, it provides the complete spectrum of amino acids, herbs, and vitamins your reproductive system needs to function optimally.
For men struggling with low semen volume due to nutritional gaps, Semenax offers a convenient all-in-one solution that supplies the missing building blocks for healthy, abundant semen production naturally.
Take Action: Correct Your Nutritional Deficiencies Today
Don’t let nutritional deficiencies continue affecting your reproductive health and confidence. Semenax provides the comprehensive nutritional support your body needs to restore optimal semen volume and overall sexual wellness.
8. Lifestyle Factors: Daily Habits That Reduce Volume 🍺

Several common lifestyle factors can significantly decrease semen volume:
Volume-Reducing Lifestyle Factors
| Factor | Impact on Semen Volume | Mechanism | Prevalence |
|---|---|---|---|
| Alcohol consumption | Moderate to significant reduction | Dehydration, hormonal disruption, nutritional deficiencies | Very common |
| Smoking/nicotine | Moderate reduction over time | Vascular damage, oxidative stress | Common |
| Recreational drugs | Variable depending on substance | Multiple mechanisms including hormonal disruption | Variable |
| Excessive heat exposure | Temporary but significant | Testicular temperature affects production | Situational |
| Sedentary lifestyle | Gradual moderate reduction | Reduced circulation, hormonal optimization | Very common |
| Poor sleep | Gradual moderate reduction | Hormonal disruption, reduced recovery | Very common |
| Obesity | Moderate to significant | Hormonal imbalance, inflammation | Increasingly common |
| Environmental toxin exposure | Variable, potentially significant | Endocrine disruption, cellular damage | Ubiquitous but variable intensity |
Evidence-Based Lifestyle Modifications 🔄
| Modification | Implementation | Expected Timeframe | Success Rate |
|---|---|---|---|
| Alcohol reduction/elimination | Limit to 0-4 drinks weekly, none before sexual activity | 2-4 weeks for initial improvement | High (70-80% report improvement) |
| Smoking cessation 🚫🚬 | Complete cessation with appropriate supports | 1-3 months for initial improvement | High when successful |
| Drug avoidance | Complete cessation with appropriate supports | Variable by substance | High when successful |
| Temperature management | Loose-fitting underwear, avoiding hot tubs/saunas | 2-3 months (sperm cycle) | Moderate |
| Regular exercise 🏃♂️ | 150+ minutes weekly moderate activity plus strength training | 1-2 months for initial benefits | Moderate |
| Sleep optimization 😴 | 7-9 hours quality sleep nightly | 2-4 weeks | Moderate to high |
| Weight management | Achieve and maintain healthy BMI | Variable based on starting point | Moderate to high |
| Environmental toxin reduction | Filter water, reduce plastics, organic foods when possible | 2-3 months | Difficult to measure but likely beneficial |
MedlinePlus provides comprehensive information on lifestyle factors affecting male reproductive health and effective intervention strategies: https://medlineplus.gov/ency/article/001954.htm
9. Stress and Psychological Factors: Mind-Body Connection 🧠
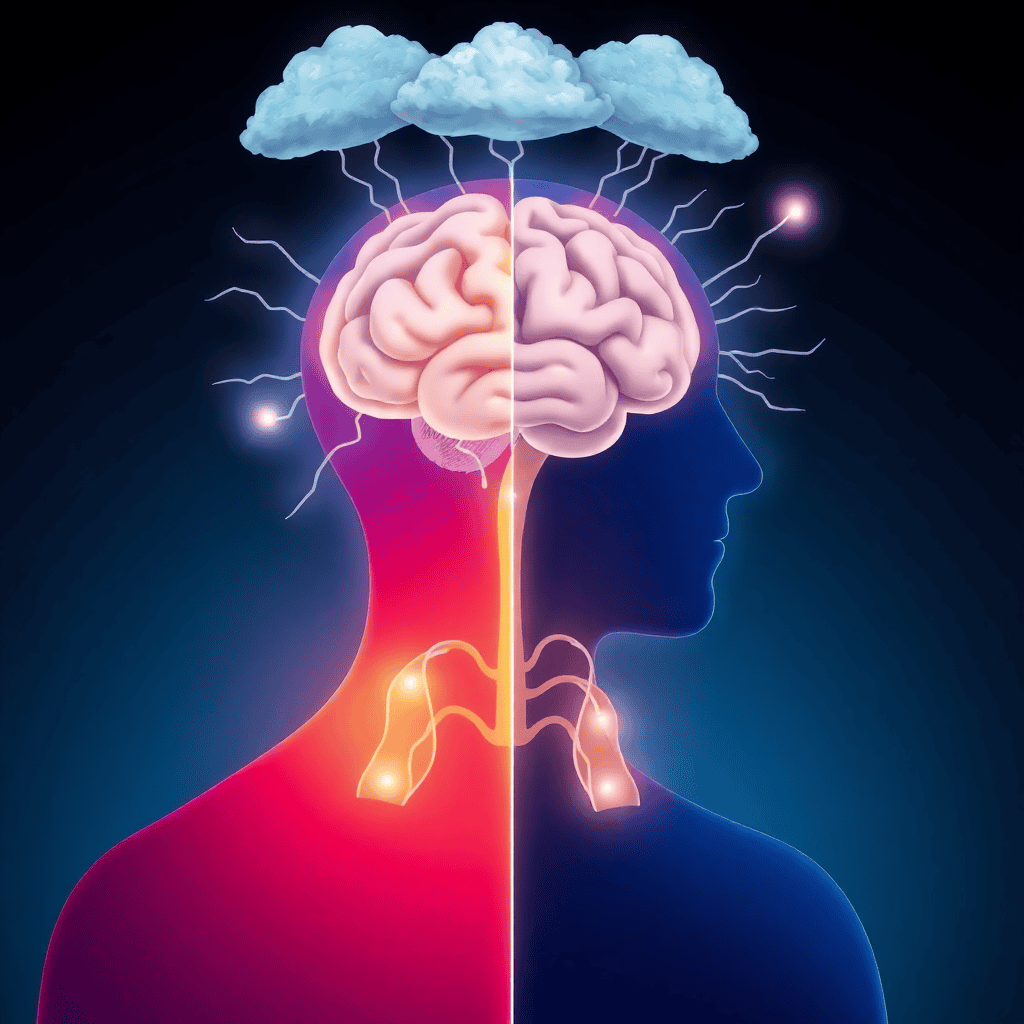
Psychological factors significantly impact reproductive function including semen volume:
Stress Effects on Semen Parameters
| Stress Type | Impact on Semen Volume | Physiological Mechanism | Related Factors |
|---|---|---|---|
| Chronic psychological stress | Moderate reduction | Elevated cortisol, suppressed testosterone | Often accompanied by sleep issues, poor lifestyle |
| Acute performance anxiety | Temporary moderate reduction | Sympathetic nervous system activation | Can affect sexual function broadly |
| Depression | Variable reduction | Hormonal imbalance, medication effects | Often accompanied by other health issues |
| Work-related burnout | Moderate reduction over time | Chronic stress response, lifestyle impact | Often unrecognized factor |
| Relationship conflict | Variable impact | Combination of psychological and lifestyle effects | May affect sexual function broadly |
| Post-traumatic stress | Can be significant | Complex neuroendocrine disruption | Often requires specialized support |
Evidence-Based Psychological Interventions 🧘♂️
| Intervention | Implementation | Expected Timeframe | Effectiveness |
|---|---|---|---|
| Mindfulness practice | 10-20 minutes daily meditation | 4-8 weeks for measurable impact | Moderate to high |
| Cognitive behavioral therapy | Professional therapy, typically weekly | 8-12 weeks for significant effect | High when appropriate |
| Stress management techniques | Various approaches (deep breathing, progressive relaxation) | 2-4 weeks for initial benefit | Moderate |
| Regular exercise for stress | 30-45 minutes 4-5 times weekly | 2-4 weeks | Moderate to high |
| Sleep improvement for stress | Consistent sleep schedule, sleep hygiene practices | 1-3 weeks | High for stress reduction |
| Social connection | Regular meaningful interaction, support systems | Ongoing practice | Moderate but significant |
| Professional mental health support | Appropriate treatment for clinical conditions | Variable by condition | High when properly matched |
The Mayo Clinic provides information on the stress-fertility connection and effective management strategies: https://www.mayoclinic.org/diseases-conditions/male-infertility/symptoms-causes/syc-20374773
10. Anatomical and Structural Issues: Physical Barriers 🧬
Some men experience low semen volume due to structural or anatomical factors:
Common Structural Causes
| Structural Issue | Mechanism | Diagnostic Approach | Prevalence |
|---|---|---|---|
| Congenital ductal abnormalities | Developmental issues in reproductive tract | Specialized imaging, examination | Rare |
| Varicocele | Enlarged veins affecting testicular function | Physical examination, ultrasound | Common (15-20% of men) |
| Ejaculatory duct obstruction | Blockage preventing normal ejaculation | Transrectal ultrasound, specialized testing | Uncommon |
| Post-surgical changes | Alteration of structures after medical procedures | Medical history, physical examination | Depends on surgical history |
| Prostate structural issues | Anatomical variations affecting fluid production | Urological examination, imaging | Variable |
Evidence-Based Management Approaches 👨⚕️
| Approach | Implementation | Success Rate | Medical Specialty |
|---|---|---|---|
| Surgical correction | Procedure specific to the condition | Variable by condition | Urology |
| Varicocele repair | Surgical or interventional radiology procedure | 60-80% improvement in parameters | Urology |
| Post-vasectomy considerations | Special approaches if related to vasectomy | Variable | Urology |
| Assisted reproductive techniques | Various medical interventions for fertility | High for reproduction but doesn’t fix volume | Reproductive Endocrinology |
| Acceptance with adaptation | Understanding permanent structural limitations | N/A | Psychological support beneficial |
Hartford HealthCare provides information on structural causes of male reproductive issues and appropriate medical interventions: https://hartfordhealthcare.org/services/urology-kidney/departments/mens-health
Conclusion: A Comprehensive Approach to Increasing Semen Volume 🌟
After examining the ten primary causes of low semen volume, several key principles emerge for effectively addressing this concern:
- Start with the Basics 💧: Hydration, abstinence timing, and basic lifestyle factors often yield the quickest and most significant improvements for many men.
- Layer Interventions Strategically 🔄: Begin with simple, non-medical interventions before progressing to more complex approaches, adding one change at a time to identify effective strategies.
- Recognize Age-Appropriate Expectations ⏳: Understanding natural age-related changes helps establish realistic goals and prevents unnecessary concern over normal variations.
- Address Multiple Factors Simultaneously 🧩: Most men with low semen volume have several contributing factors, making a comprehensive approach most effective.
- Seek Medical Evaluation When Appropriate 🩺: Persistent issues, especially when accompanied by other symptoms or fertility concerns, warrant professional medical assessment.
- Balance Volume Goals With Overall Sexual Health ⚖️: Focus on comprehensive sexual wellness rather than fixating exclusively on volume as a measure of sexual adequacy.
For most men concerned about semen volume, a systematic approach addressing hydration, nutrition, lifestyle factors, and stress management will yield noticeable improvements within 2-3 months. However, when these interventions prove insufficient, medical evaluation can identify and address underlying conditions requiring specialized treatment. By understanding these common causes and their solutions, men can effectively address low semen volume while improving their overall reproductive and sexual health.
